How to Overcome Emotional Eating
Do you find yourself reaching for a slice of chocolate cake when you’re feeling down?

As you sink your teeth into the creamy icing – dopamine (the feel-good hormone) gets released into the brain, making you forget your troubles for just a split second. The feeling is good enough that your body learns to crave and long for something sweet and sugary every time you feel upset or angry.
Sound familiar? Well, this is what we call emotional eating. Emotional eating is when you rely on food to help you deal with your emotions instead of eating when you actually feel hungry.
And while I’m sure that every one of us has finished a tub of ice cream or an entire bag of chips in one sitting, it’s probably fair to say it only happens on occasion. Emotional eating, on the other hand, happens more consistently and often leaves you feeling guilty for, once again, overindulging.
If you find yourself mindlessly eating when dealing with your emotions, you’re not alone. According to an Australian study, emotional eating affects 83 per cent of people who struggle with their weight.
Let’s look at the importance of our relationship with food and its impact on our health.
Unhealthy relationships with food
The relationship one forms with food early on in life can greatly impact how food is viewed as an adult. Childhood eating habits and patterns often continue into adulthood and are a strong determinant as to why we are facing an obesity epidemic today.
Of course, we all have our favourite childhood sweets or ice creams that bring back memories of summers spent at the beach.
But when we become dependent on fatty, fried or sugary foods to feel better, we run into a myriad of problems.
To give you an example of how unhealthy eating patterns can stem from one’s childhood – picture this:
A 5-year-old child is given a double chocolate chip cookie every time he cries. Understandably, this child starts to associate a chocolate chip cookie as somewhat of a reward or treat that makes him instantly feel better.
This carries on throughout his childhood; every time he cries, his parents give him something that tastes good to stop him crying.
Subconsciously, this child develops a behaviour that carries through to adulthood. Every time he struggles to deal with his emotions, he goes to the cupboard and grabs a chocolate bar or doughnut.
Not only is this bad for his health, but it is also an ineffective way to deal with emotions.
Before we move on, it’s also important to note that emotional eating is not only associated with negative feelings. Many people also view unhealthy foods as a ‘reward’ for something they’ve achieved or feel good about. Again, this is OK now and then! But when it happens regularly, the problem ought to be addressed.
So, as we can see, one’s upbringing plays a powerful role in relationships with food. So, how can one overcome an issue that has stemmed from childhood and seems to be an ingrained lifestyle? Well, the first step is awareness. Only when one becomes aware of their behaviour can they can actively work to change it.
Overcoming Emotional Eating
As we now know, feeding emotions with comfort foods is a coping mechanism developed over time. Therefore, it’s no surprise that to overcome emotional eating, time and dedicated effort are required. However, if you’re committed to breaking your emotional eating habit, here are some healthy tips to help you see food in a new light.

1. Create an ‘emotion’ diary
Use a diary and note down the feelings and emotions that lead you towards the snack cupboard. Writing notes in a food diary can help you find links and patterns between your feelings and behaviours. For example, perhaps you find you end up eating unhealthy food whenever you fight with your partner or when you get in trouble at work.
This is the first step towards self-awareness and will help you understand your triggers.
Once you’ve identified these triggers, you empower yourself to regulate your responses to them. In addition to noting down your emotions that lead to emotional eating, you can also write down the foods you eat.
Identifying these patterns can help you recognise when you emotionally eat.
2. Follow the ‘5-minutes off’ rule
Every time you find yourself craving specific foods at vulnerable moments, give yourself five minutes off.
Step away from what you might be doing at that time and allow yourself an entire five minutes to reflect on how you are feeling, and ask yourself these questions:
-Am I hungry or do I want to eat because I’m feeling stressed or low?
-Am I using food as a way of rewarding myself? If yes, how often do I do that?
-Can I swap the unhealthy food with something healthy, but something that also tastes good?
Asking these questions will help you understand what your body really needs while also giving you time to re-think impulsive behaviours (like eating unhealthy snacks every time you feel emotionally charged up).
3. Steer clear of unhealthy foods

While this might sound too simple – it’s one that works. Clearing out your kitchen cabinets and re-stocking them with healthier snacks can help you keep calories at bay.
The best way to have no unhealthy foods in the cupboard is to not purchase them at the supermarket.
This is a great strategy for changing your habits. Once you start doing this, you will uncover a whole world of healthy, tasty snacks. Your taste buds will also adjust too, and you’ll start to indulge in the flavours that healthy foods have to offer.
Before you set out on your journey to overcome emotional eating, it’s important to note that it’s not a task that can be achieved in one day.
It will take some time to rewire yourself emotionally, but it will definitely be worth it.

Every time you feel the urge to grab a decadent dessert or a salty snack to cheer yourself up when you are feeling low – remind yourself that you are bigger than your cravings. Reaffirm your belief in yourself and find alternatives.
It’s likely you’ll slip up from time to time, but the important thing is to make small adjustments and improvements.
Try tuning in to your body, understand its needs and start eating only when you feel hungry.
And lastly, if you make mistakes, tell yourself that it’s okay, but do your best to put yourself back on track. After all, we are all human. But you’ve got to be dedicated – find that will power and fight inside of you to overcome emotional eating and develop a better relationship with food.
However, willpower alone won’t address the inner conflicts associated with food and managing challenging emotions.
Feel free to speak to one of our professional therapists for Emotional eating treatment . You can link up through a confidential and secure video conferencing session – anywhere in Australia or call 03 9557 9113 for an appointment in our Melbourne clinic. Professional help is just a click away. All you need to do is reach out.
Here are a couple of blogs written on this topic you might find useful:
What Are Australians Most Afraid Of? N...
From snakes and spiders to needles and ghosts, fear takes many forms. But what do Australians fear most in 2025? At Bayside Psychotherapy, our expert.
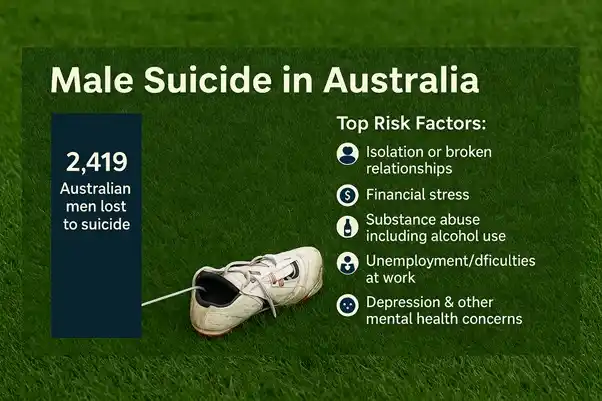
Is It Time For The AFL To Cast A Menta...
At Bayside Psychotherapy we are passionate about mental health and like many fellow Melbournians, many on our team are avid AFL fans. So when two of our.
Exploring Emerging Therapies: Understa...
At Mind Medicine Australia, we are dedicated to transforming the trea.
The Balance of Power in Romantic Relat...
Why do some relationships thrive while others feel like a constant tug-of-war? Power dynamics lie at the heart of this balance.