Mindfulness Meditation in therapy by Adam Szmerling
MINDFULNESS THERAPY
Mindfulness is a relatively modern phenomena in the world of psychotherapy, emerging from the Eastern contemplative traditions. While most commonly associated with mindfulness meditation, mindfulness therapy involves an acute perception of moment by moment experience (Shapiro, Carlson, Astin & Freedman, 2005). Epstein (2005) proposed an intense and obsessive desire for change in external or internal circumstances creates suffering rather than the desired goal state. Gilligan (1997) argues this strong and impatient yearning stems from Western cultures progressively heightened obsession with consumerism and speed of service. Consequently, the potential for happiness to be generated from within has been oversighted. Mindfulness can gradually lessen these intense fixations, and cultivate authentic and lasting happiness (Epstein). This facilitates one’s ability to experience the completeness of life and engage in the myriad of human emotions and sensations as they unfold from moment to moment. When life is experienced from a non-judgemental stance and based in the present moment, one’s ability to form stable, non-reactive responses to distressing situations increases (Ott, Norris & Bauer-Wu, 2006).
MINDFULNESS APPLICATIONS IN PSYCHOLOGICAL ILLNESS
Kabat Zinn (1990; cited in Kostanski & Hassed, 2008) was instrumental to the integration of mindfulness into the domain of psychology and psychotherapy. He developed the Mindfulness Based Stress Reduction (MBSR) program. The MBSR program involves eight weekly 2.5hr group classes during which four mindfulness techniques are presented and imparted. The first is a body scan whereby participants gradually move their attention to each body segment from toe to head. Secondly, hatha yoga where slow and gentle stretching enhances body awareness and flexibility. The third and fourth are sitting and walking meditation respectively, which are both traditional forms of meditation. Participants are given guided audio tapes to facilitate daily independent practice of the body scan, yoga and sitting meditation. Homework comprised the recording of pleasant and unpleasant events and the correlating thoughts and feelings. Group sessions also involve discussions and tools to improve communication, coping strategies and disrupting unhelpful habitual behaviours (Koerbel & Zucker, 2007).
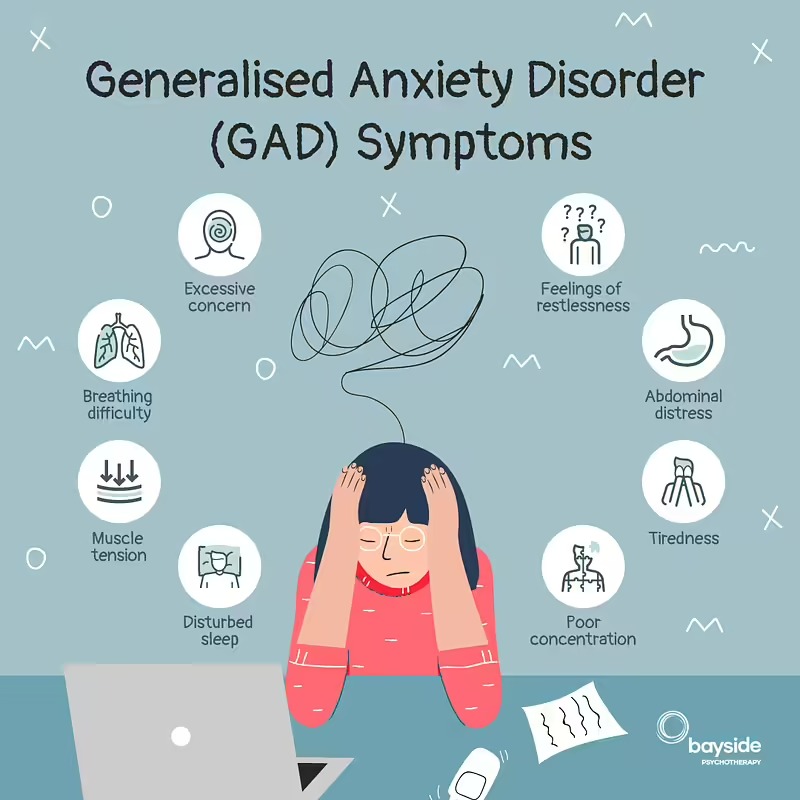
Jain, Shapiro, Swanick, Roesch, Mills, Bell and Schwarz (2007) investigated whether mindfulness meditation techniques (MMT) or somatic relaxation (SR) techniques were more efficacious in reducing psychological symptoms in 83 stressed university students over four weeks. The MMT was based on the MBSR program and involved four 1.5 hour weekly sessions during which subjects learned the MBSR program components. SR participants were taught progressive muscle relaxation, imagery and breathing techniques. Both groups were given homework and tapes to support independent practice. The mean pre-test score on the Global Severity Index (GSI) indicated participants were experiencing substantial psychological distress. While both MMT and SR were more effective in reducing psychological distress compared to no intervention, MMT was superior in diminishing ruminative and distractive thoughts. Only the MMT participants mean GSI score fell to within normal parameters, suggesting MMT hold specific benefits for clinical problems.
Mindfulness also appears to resolve residual symptoms in those with major depressive disorders. Kingston, Dooley, Bates, Lawlor and Malone (2007) investigated the effectiveness of mindfulness, in combination with cognitive therapy, in treating depressive relapses in 19 psychiatric outpatients who had experienced three or more depressive episodes. Two of the authors taught the mindfulness components during the 2-hour group sessions over eight weeks including formal mindfulness meditation training, body scanning and mindfulness movement training. Results indicated depressive symptoms diminished during and after the mindfulness program. Although two of the authors delivered the psychological treatment to participants, no ethical issues were identified.
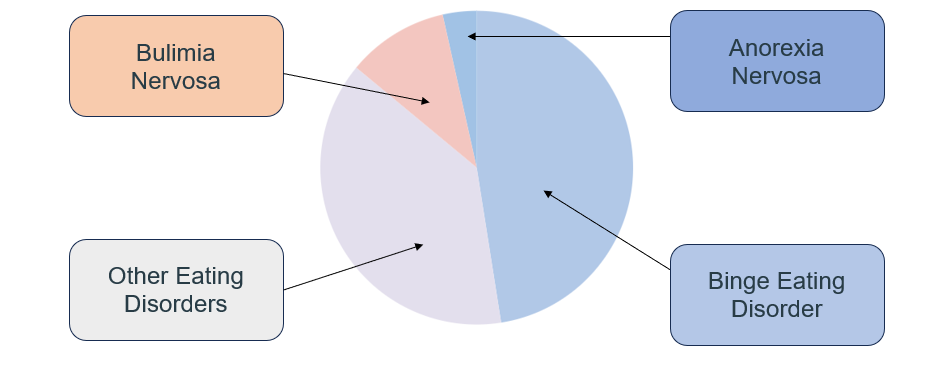
Further support for mindfulness techniques in psychology has been shown in the area of eating disorders. Smith, Shelly, Leahigh and Vanleit (2006) investigated whether a MBSR program modified to specifically address eating patterns could reduce binge eating behaviour. Participants included binge eaters and non binge eaters. While subjects who did not binge previously demonstrated unchanged eating patterns, those classified with mild or moderate binge eating disorder demonstrated a moderate to large significant change in their eating patterns. A relationship between less binge eating and increased self acceptance and lower state anxiety was also established, which suggests mindfulness interventions lower depressive and anxious symptoms. Similar findings were reported by Kristeller and Hallett (1999) who also explored whether mindfulness influenced binge eating behaviour in 18 obese females. Mindfulness interventions included general mindfulness meditation (attending to thoughts, emotions and body sensations but focusing on the breath primarily), eating meditation (attending behaviours, beliefs and emotions concerning food) and mini-meditations (focusing on thoughts and feelings for a few minutes prior to meals and binge episodes). Seven group sessions were held over six weeks. Participant’s binge eating episodes reduced from a mean of 4.02/week pre-treatment to 1.57/week post-treatment; depression and anxiety levels also fell significantly.
LIMITATIONS OF CURRENT RESERACH
It is clear that evidence exists to support the use of mindfulness in treating psychological problems including anxiety, depression, stress and binge eating. In all of these pathologies, mindfulness appears to promote self-regulation and enhance insight and the integration of emotional, cognitive, physiological and behavioural facets of human functioning (Kristeller & Hallett, 1999). However, limitations are apparent in the existing research. Mindfulness techniques appear effective in group therapy settings, however an exploration of their application to individual therapy has not occurred. Additionally, the influence of gender on psychological distress levels following mindfulness interventions is unclear. Some studies have included only female participants (Kristeller & Hallett, 1999), whilst others have involved samples comprised of substantially more females than males (Jain et al., 2007; Kingston et al., 2007; Smith et al., 2006). It is interesting that of the three possible mediators in the relationship between mindfulness and psychological distress (emotion regulation, equanimity and rumination), rumination is frequently used as a coping strategy in females. Rumination however is positively correlated with depressive symptoms (Nolen-Hoeksema, Morrow & Frederickson, 1993; cited in Thayer, Rossy, Ruiz-Padial & Johnsen, 2003).
Thayer et al. (2003) found that females ruminated and thought more about their emotions and behaviours than men. Additionally, in comparison to highly depressed men, highly depressed females tended to ruminate more, were less able to regulate negative emotions, and experienced depression more intensely. Nolen-Hoeksema and Jackson (2001) proposed the greater incidence of rumination in females explains why they experience depression more than males. This is possibly due to the emotion coping strategies conditioned in male and female children. Whilst females are encouraged to express emotions relating to fear and sadness, males are discouraged to outwardly express such emotions. This can lead to females having greater emotional awareness and expressiveness, but can also foster maladaptive behaviour if ruminative tendencies are generated. In contrast, males are encouraged to manipulate and control their environment in an attempt to regulate their emotions.
A highly recommended book on Mindfulness is Full Catastrophe Living.
Here are a couple of blogs written on this topic you might find useful:
Choosing the right therapist: The 5 mo...
Choosing the right therapist can be difficult. Different problems and diff.
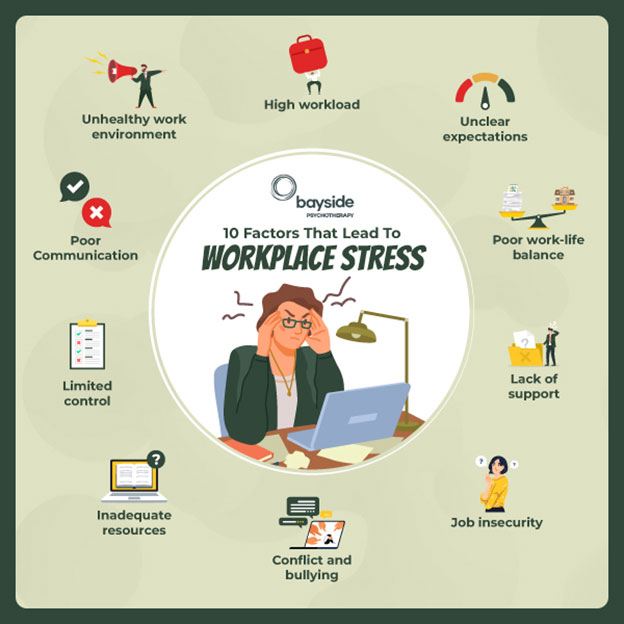
Creating Healthier Workspaces: How str...
Employee mental health is pivotal to overall workplace wellbeing, impacting individual performance, job satisfaction, and organ.
From High Stakes to Healing: 8 Tips To...
Gambling activities have become more accessible and convenient due to the proliferation of casinos and the rapid growth of online gambling platforms. Mo.
An Examination of Bulimia Nervosa Amon...
Bulimia nervosa is a serious eating disorder that can significantly impact an individual's physical and psychological health. Characterised by recurrent.