
What Is Trichotillomania?
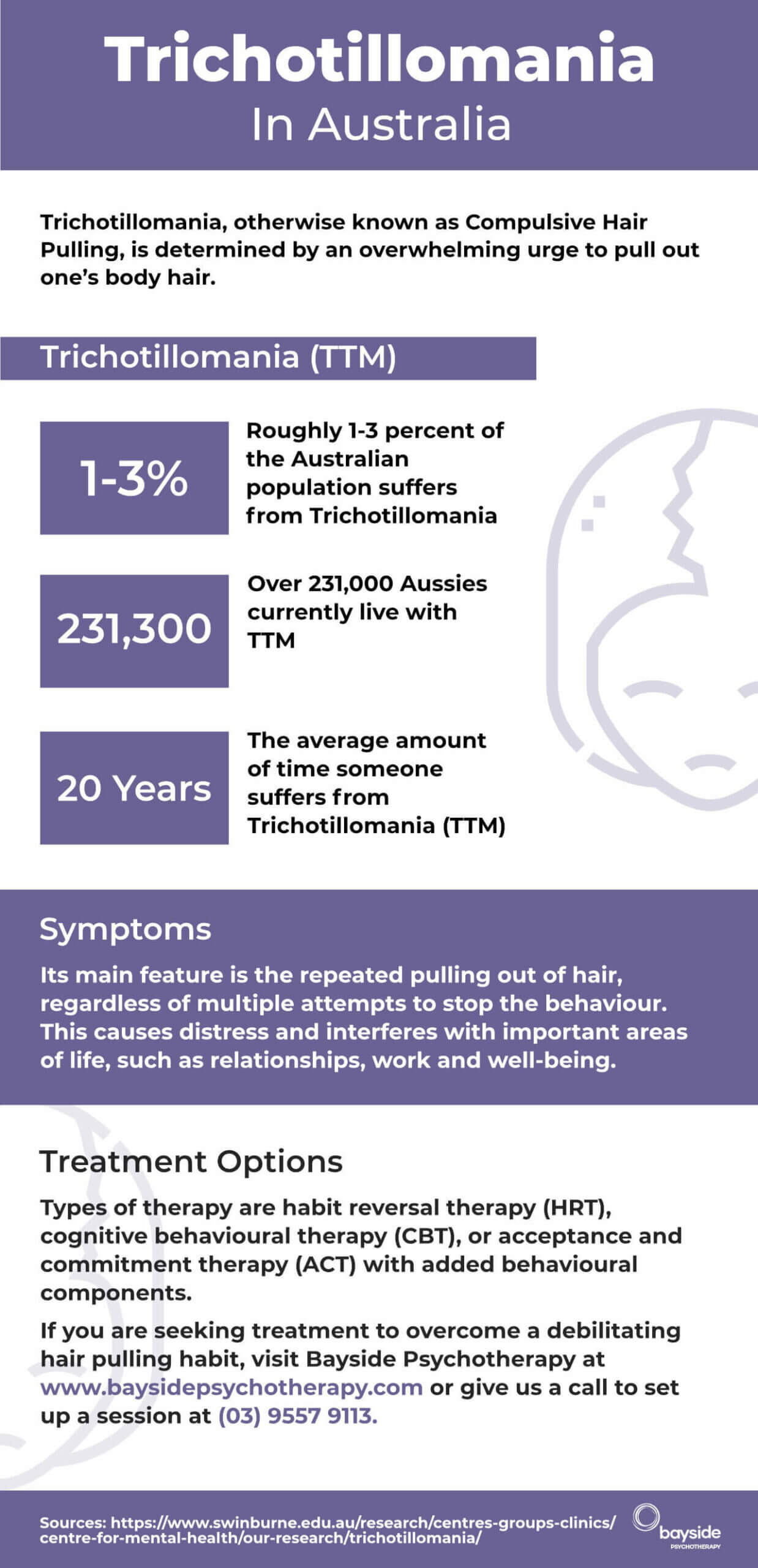
Trichotillomania, or compulsive hair pulling, is a condition where people feel a strong urge to pull out their hair. Although first noted in 1889, it was only recognised as a disorder in 1987. Trichotillomania is often referred to as ‘trich’ for short. Today, it affects around 2–4% of Australians, often starting in adolescence.
Many who suffer feel ashamed or embarrassed, keeping it hidden from loved ones. You’re not alone, and help is available.

What Are The Symptoms Of Trichotillomania?
Common signs include:
- Recurrent hair pulling leading to visible hair loss, such as thinning eyebrows or bald patches in specific areas of the scalp or other regions where thinning occurs.
- Struggling to stop despite conscious efforts.
- Feeling tension, anxiety or boredom before pulling, followed by relief or satisfaction afterwards.
- Skin damage from repeated pulling, including scabs or scars.
If this sounds familiar, we recommend consulting with one of our experienced therapists for support.
What Causes Trichotillomania?
Hair pulling often serves as a way to cope with stress, boredom and anxiety, providing temporary relief. It can co-occur with depression or other repetitive behaviours like nail-biting. Shame, guilt and suppressed anger are also common.
Research links early trauma or abuse to the development of trichotillomania in some cases. However, every person’s experience is unique.
Trichotillomania-related hair loss is sometimes mistaken for alopecia, but the causes and treatments for these conditions are different.

What Are The Current Treatment Options?
Cognitive Behavioural Therapy (CBT) or psychodynamic therapy:
CBT is the most common treatment for trichotillomania and aims to help individuals recognise and understand the triggers behind their hair-pulling disorder. A Cognitive Behavioural Treatment program can teach a person strategies to manage the urge to pull their hair. Habit Reversal Training (HRT) is often used to help control the physical and psychological symptoms.
Psychodynamic therapy on the other hand is deeper, insight oriented aiming to address childhood conflicts and unprocessed memories that may have led to trichotillomania forming.
Joining A Support Group:
Joining a support group of other people with trichotillomania can be an indispensable source of support, understanding, coping techniques and ways of treating trichotillomania.
Relaxation Techniques:
Methods such as meditation, deep breathing exercises, and progressive muscle relaxation can help reduce repetitive behaviours by managing the underlying stress or anxiety that the urge to pull hair causes.
Need trichotillomania therapy?
Start Now
Seeking Treatment For Hair Pulling With Bayside Psychotherapy
Get in touch with us through our online contact form
Call Bayside Psychotherapy on (03) 9557 9113 to find out if we’re able to help you. Your call is completely confidential, and there’s absolutely no obligation.
You can also book an appointment by using our online booking form for online appointments. Or, if you prefer, you can book an in-clinic session.
Self-hypnosis may also work well when used in conjunction with counselling. You can download our Hair Pulling Self Hypnosis recording from our website.
Does Treatment Take Long For Compulsive Hair Pulling?
Results vary based on your readiness and commitment. Long-term sufferers may need more time, but many find improvement with consistent therapy and support.
Call us today on (03) 9557 9113 or use our contact form to find out if we can help you work through the compulsion to pull your hair. Your call is completely confidential, and there’s absolutely no obligation.
There’s also the option to book an appointment now, for online or in Melbourne therapy.
Note: This information is informative only and is not to be used for diagnosis or substitution of appropriate assessment and/or treatment by a registered practitioner. Information on this page and our entire site should not be construed as implying that our therapists are specialists in treating any condition whatsoever. While some of our therapists may have experience working with people suffering from a specific condition, not all of our therapists do. We do not guarantee any particular level of performance, cure or management of symptoms. Each case is unique and responds differently with collaboration between client and therapist being crucial. Always seek an appropriate assessment from a qualified professional such as a GP, psychiatrist, clinical psychologist or social worker especially if you are acutely distressed.








